Have You Ever Wished Your Doctor Could Feel Your Pain?
I’ve lost count of how many times I’ve sat across from a doctor, trying to explain what my body feels like on a daily basis. Shooting pains down my legs. Brain fog so thick I forget what I’m saying mid-sentence. The kind of exhaustion that doesn’t go away with sleep. And every time I try to describe it, I get the same blank stare… followed by, “Maybe some light exercise would help.”
That’s usually the moment when I imagine how satisfying it would be to have a little device that could transfer pain to my doctor. Just temporarily. Just enough for them to get it. Not to be cruel—just to create understanding. Because once you feel what someone else is living with, you stop minimizing it. You stop blaming it on stress or saying things like, “You’re probably just tired.”
This thought always hits me hardest after reading something like Living with Chronic Pain and Fatigue – What Nobody Sees. Because it’s true—so many of us are hiding behind smiles, surviving on painkillers, caffeine, and hope… just waiting to be heard.
The Concept: A Shock Collar for Medical Empathy
Let me walk you through my imaginary invention. Picture this: a small, wearable device that syncs to your nervous system. When your symptoms spike, you press a button and BOOM—your doctor feels a wave of exactly what you’re going through.
Your lower back pain when lying down? Transferred.
Your nausea and dizziness after a shower? Sent.
Your fiery leg cramps at night? Delivered directly.
For fun, there’d be different settings. “Fibro flare level 5.” “Sciatica simulator.” “Stomach spasm mode.” I’d name it something catchy like the “EmpaTech”—short for Empathy Technology. Patent pending, of course.
Jokes aside, there’s something powerful about the idea. I’m not asking for my doctor to suffer. I’m just tired of suffering alone. If even for five minutes, they could feel that deep gnawing ache I get in my lower spine, maybe they’d stop suggesting I “stretch it out.”
Like when I tried to explain how laying down flat makes my back pain even worse, and the doctor just said, “That’s unusual.” As if I haven’t been living with that pain for years.
Why So Many of Us Feel Misunderstood by Doctors
It’s exhausting enough dealing with chronic pain. But trying to explain it to someone who doesn’t believe you—or worse, blames you for it—is next level. I’ve been told it’s anxiety. I’ve been told I just need to lose weight. I’ve been told my labs are fine, so “it can’t be that bad.”
But here’s the thing: chronic conditions like fibromyalgia, nerve pain, IBS, or autoimmune issues don’t always show up on blood tests. That doesn’t make them any less real.
When doctors treat symptoms like they’re imaginary, it can destroy your confidence. You start doubting yourself. You feel crazy. It becomes harder and harder to advocate for your health when the people you turn to for help act like you’re exaggerating.
This is where we desperately need compassion in care. Until then, maybe my “EmpaTech” can bridge the gap.
And when the stress of being dismissed turns into insomnia, racing thoughts, or panic attacks, I’ve had to learn how to self-soothe. One of the best tools I’ve come across? Calming an overactive nervous system naturally. Because some days, that’s the only thing keeping me sane.
It’s Not Laziness. It’s Reality.
People love to throw out advice when they don’t understand what you’re going through. “You just need to push through it.” “You’d feel better if you exercised more.” “Maybe you’re just depressed.”
What they don’t see is what happens after I take a shower and try to clean the kitchen—dizziness, nausea, and stabbing pain that forces me to lay down for an hour. I’m not being lazy. I’m surviving.
When you’re living with chronic fatigue and pain, even the simplest tasks feel like climbing uphill with a weighted vest. That’s why I connected so deeply with the stories shared in Chronic Fatigue Recovery Stories. Reading how others navigate this storm gave me permission to stop blaming myself.
And honestly, if doctors could feel even one afternoon of what we endure daily, they’d stop treating it like we’re just “tired.” That’s why my imaginary pain-transfer device should be standard issue in med school.
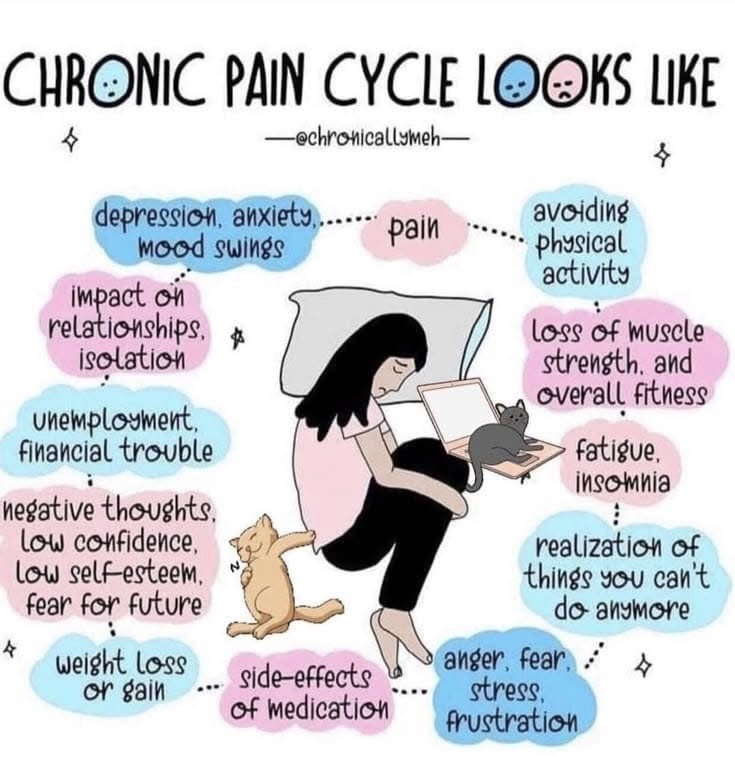
The Chronic Pain Cycle: A Vicious Loop Nobody Sees
The worst part about chronic illness isn’t just the physical pain—it’s the chronic pain cycle it traps you in. One symptom triggers the next like falling dominoes:
- Pain →
- Fatigue →
- Insomnia →
- Anxiety →
- Depression →
- Isolation →
- More pain…
And repeat.
This isn’t just theory—it’s my life. There have been times I didn’t leave the house for days because I was too sore to walk or too emotionally drained to talk to anyone. That cycle is real, and it wears down even the strongest people.
That’s why I love the visual that inspired this article. The one where side effects compete with symptoms and “good” days still include pain and fatigue. If you’re nodding your head while reading this, you’re not alone. I’ve been in that exact place—many times.
When I hit my lowest, I started digging for anything that could help, even a little. That’s when I found the idea of addressing deeper physical issues, like how a hiatal hernia might be adding to my pain and discomfort. Every layer you can address matters.

Doctors Mean Well—But the System Doesn’t Always Help Us
Look, I don’t think most doctors are trying to be cold. The system they work in is built for quick visits, prescription pads, and lab results—not complex, long-term suffering. They don’t have the time, tools, or sometimes even the training to deal with things like fibromyalgia, ME/CFS, or chronic Lyme.
So we end up bouncing between appointments, referrals, and scans—desperate for someone to really listen. I’ve cried after leaving appointments where I felt ignored or brushed off. It’s why I’ve started tracking everything myself, journaling symptoms, and being extra specific, hoping that maybe this time, they’ll understand.
Wouldn’t it be easier if I could just push a button and transfer my symptoms over, just for 60 seconds?
That might do more for diagnostics than all the MRIs and lab work in the world. Because as you probably know from reading Why Does My Back Hurt When I Lay Down Flat?, pain doesn’t always show up where or how you’d expect.

Chronic Pain Isn’t One-Size-Fits-All
That’s another thing I wish more doctors—and honestly, more people in general—understood. Chronic pain doesn’t look the same from person to person. Some people feel it deep in their joints. Others have stabbing nerve pain. Some can’t sleep. Some can’t eat. Some can’t even think straight.
For me, it’s a mix of everything: neck and shoulder pain, lower back issues, that deep burning in my left leg, and sometimes even chest discomfort. It feels like my body is constantly trying to send out an SOS signal—and nobody knows how to answer it.
I used to feel like I had to downplay it, but not anymore. I’ve learned to say it plainly. The pain is real, it’s complex, and it deserves attention. If you’re reading this and nodding your head, that means you deserve it too.
Reading through real talk like Living with Chronic Pain and Fatigue – What Nobody Sees reminded me I’m not being dramatic. I’m just finally being honest.
When Your “Good” Day Still Includes Pain
You know what really gets me? When someone says, “You look like you’re feeling better today!” And I just smile and nod because explaining that I’m still in pain—but just hiding it better—feels like too much.
Chronic illness trains you to perform wellness. You laugh through joint stiffness. You carry on conversations while your stomach cramps. You attend events, then crash for three days afterward.
That’s what people don’t see. Even on my “good” days, I’m measuring every step I take. How long can I stand before my back tightens up? Will this chair trigger my sciatica again? Can I even drive myself home?
It’s this invisible balancing act that you get used to—but it’s not easy. And it’s definitely not overthinking. I’ve even had to start using support tools, like a lumbar support pillow for sleeping, just to get a couple hours of decent rest.

The Fear of Losing Who You Used to Be
This one is hard to talk about—but it’s real. When you live with chronic pain or illness for long enough, you start to grieve the person you used to be. I miss being able to hike, to clean the house without crashing afterward, to plan things without worrying I’ll have to cancel.
That loss hits deep. It’s not just about activities—it’s about identity. I used to feel strong. Capable. Independent. Now, I feel like a different version of myself. A version that needs help more often. A version that cancels plans. A version that has to think about every single movement.
But even in that grief, there’s power in acknowledging it. Talking about it. Validating it. I’ve found healing not in pretending I’m okay—but in connecting with others who get it. Who really get it. Like in chronic fatigue recovery stories—they reminded me I’m not broken. I’m adjusting. Adapting. Still here.
We Deserve Compassion—Not Just From Others, But Ourselves
If there’s one thing I’ve learned through all this, it’s that compassion has to start with us. We spend so much time wishing doctors would understand, hoping our friends would check in, and trying to make people see that our pain is real.
But sometimes, the first person who needs to hear that truth… is us.
You’re not weak because you’re tired. You’re not lazy because you need to rest. You’re not dramatic because you’re still in pain from doing something “normal.”
You’re living with something hard—every single day. And you’re still here. You’re reading, researching, trying, surviving.
That’s not failure. That’s strength.
If you’ve ever felt like you were going crazy because no one around you understands, let me just say: I see you. You’re not alone in this. There’s a whole world of people like us trying to hold it together through pain, fatigue, brain fog, and everything in between.
And the more we speak out, share what this chronic pain cycle is really like, and connect over shared experiences—whether it’s through articles like How to Calm an Overactive Nervous System or just venting with a friend—the more hope we create.
Even if the system is slow to change, we can still show up for each other. And for ourselves.
As an Amazon Associate we earn from qualifying purchases through some links in our articles.